Trigger Points
Table of Contents
Definition
- Trigger Point (TrP) is the hyperirritable point, a palpable nodule in the taut bands of the skeletal muscles’ fascia.
- straight compression or muscle contraction can evoke a jump sign, local tenderness, local twitch response & referred pain which commonly responds with a pain pattern different from the spot.
- Jump sign is the particular behavioral response to pressure on the TrP.
- Individuals are often startled by extreme pain. They wince or cry out with a response seemingly out of proportion to the respective pressure exerted by the examining digits. They move involuntarily, jerking the head, shoulder, or another body part not being palpated.
- A jump sign thus reflects the intense tenderness of the TrP.
- This response has been considered pathognomonic for the presence of TrPs.
- The low twitch response is Called a palpable contraction of the muscle palpable, transient visible, and skin as the tense muscle fibers contract when pressure is applied through needle penetration or by transverse snapping palpation.
- A local twitch response on stimulating active TrPs is a largely confirmed diagnostic sign.
- Referred pain, also called reflective pain, is pain perceived at a location different from the place of the painful stimulus. Pain is reproducible & doesn’t have myotomes, dermatomes, or nerve roots.
- There is no certain joint swelling or neurological problem. Pain from a myofascial TrP is a distinct, discrete, and constant pattern or map of pain with no sex or racial differences able to reproduce symptoms – referred pain map.
- Radiating pain is slightly different from referred pain; for example, the pain related to a myocardial infarction could be the referred or radiating pain from the chest.
- Referred pain is when the pain is located differently or adjacent to the organ involved; for example when a person has pain only in their jaw or left arm, but not in the chest.
Anatomy and causes
- Trigger points exist in the myofascial, mostly in the center of a muscle belly where the motor endplate enters (central & primaryTrPs).
- Those are palpable nodules inside the tight muscle at the size of 2-10 mm and can indicate distinct places in any skeletal muscles of the body.
- We all have TrPs within the body. Can be present in children and even in babies, but their presence does not important result in the formation of pain syndrome.
- When it happens, TrPs are precisely related to somatic dysfunction, myofascial pain syndrome*, restricted daily functioning, and psychological disturbance
- Myofascial Pain Syndrome refers to regional pain of soft tissue origin and is related to muscle tenderness that comes from TrPs, focal points of tenderness, a few millimeters in diameter, found at various places in a muscle and the fascia of muscle.
- etiology – commonly, TrPs happen due to:
- Aging,
- Injury sustained by a fall, .by stress, or birth injury
- Lack of exercise – usually in sedentary persons between 27,5-55 years, of which 45% are male,
- Bad posture – upper and lower crossed pattern, swayback posture, cross-legged sitting, telephone posture, ,
- respective micro-trauma and Muscle overuse – weightlifting,
- Chronic stress conditions – depression, anxiety, psychological stress trauma,
- Vitamin deficiencies -folic acid; iron; vitamin C,D,B,
- Sleep CYCLE disturbance,
- Joint problems and hypermobility.
Classification of TrPs
TrPts can be separated into several groups:
- Primary
- Satellite Trigger Points
- Central and Secondary
- Primary or Central TrPs are those that cause extreme pain locally at the pressure with irradiation related to referred pain map.
- commonly are based surrounding the center of a muscle belly.
- Secondary or Satellite TrPs comes in response to the present central trigger spot around muscles.
- They commonly spontaneously take back when the central trigger point is healed. Can exist in the form of a group.
- Active and Inactive /Latent Trigger Points
- Active TrP is any spot that causes tenderness and referred pain when palpation. Palpation may also result in autonomic symptoms example dizziness, skin redness, and sweating, Latent TrP does not elicit pain spontaneously, and local or referred pain occurs only with powerful digital pressure.
- They may alter muscle activation patterns or cause muscle weakness in pain-free patients. Reproduction of pain is a diagnostic criteria differentiating between the two.
- Diffuse Trigger Points usually occur in case of extreme postural deformity where initially primary TrPs are in multiple, so secondary multiple TrPs are only a response of a mechanism, known as diffuse.
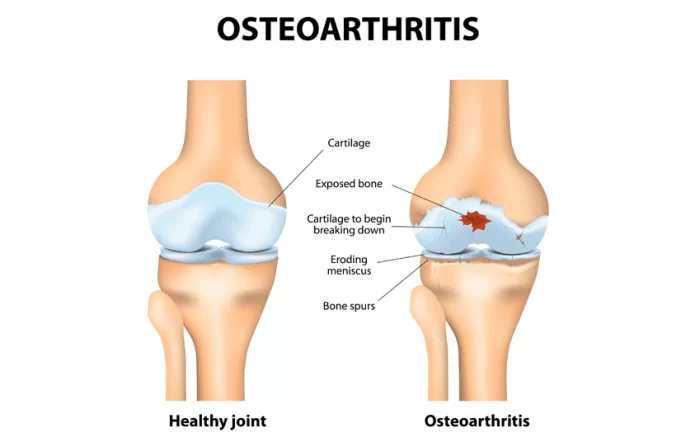
- Attachment Trigger Points come in tendon-osseous junctions which result in very tender. If not treated, degenerative processes of a neighbor joint can spring up.
- Ligamentous Trigger Points Even ligaments can result in trigger points.
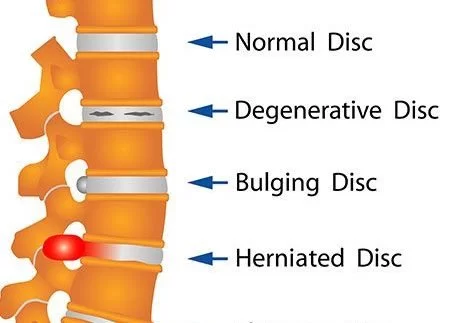
- The presence of TrPs in the anterior longitudinal ligament of the spine can cause neck instability. certain knee pain syndromes are successfully treated when treated fibular collateral ligament and ligamentumpatellae.
- Pathogenesis and Theories Little is called about the development of TrPs. There are certain theories written in the literature that try to define the development, sensitization, and manifestation of TrPs, but few of them have a powerful indication.
- Under normal conditions, pain from TrPs is mediated by unmyelinated (C) fibers and thin myelinated (Ad) fibers. distinct noxious and innocuous events, for example, chemical mediators and mechanical stimuli, may excite and sensitize Ad fibers and C fibers and thereby play an important role in the formation of TrPs.Integrated Trigger Point
- Hypothesis (ITPH) is the existing working theory. When sarcomeres and motor endplates become hyperactivated for a number of distinct causes, pathological changes begin at cellular levels. which turns on permanently sarcomeres resulting in a local inflammatory response, lack of oxygen supply, lack of nutrient supply, endogenous (involuntary) contraction of muscle fibers, and enhanced metabolic demand on local tissues.
- Electrophysiological investigations of TrPs display phenomena which indicate that the electrical activity comes from dysfunctional extrafusal motor endplates instead of muscle spindles.
- The polymodal hypothesis defined the presence of polymodal receptors (PMRs) all over the body which under some constant, pathological stimuli result in trigger points.
- Radiculopathy theory defined a straight relationship between problems on the nerve roots which result in local and different neurovascular signals and trigger points creation. Peripheral and Central Sensitization – Central sensitization is the phenomenon, together with peripheral sensitization, which helps in understanding chronic or amplified pain.
- There is central sensitization after an extreme or repetitive stimulus of the nociceptor present in the periphery, resulting in a reversible enhancement of excitability and of the synaptic efficacy of central nociceptive pathway neurons.
- Manifested as overactivated of the pain (known as hyperalgesia secondary to puncture and tactile allodynia or pressure). These CNS changes may be detected by imaging techniques or electrophysiology
Differential Diagnosis
Fibromyalgia –
- It is defined by diffused fatigue and aches throughout the body. common in women, does not affect joints but does associate with all other tissues (ligaments, muscle, tendon, bone, and fat), and can foam tender points.
- Tender points are a different place of tenderness over soft tissues that result in local pain and are tender to palpation but patients do not present jump signs when pressed nor referred to pain maps.
- These two pain syndromes may overlie in symptoms and are hard to differentiate without a thorough assessment by even a skilled physician. Although they may be concomitant and may communicate with each other.
- Other conditions which involved muscle pain and trigger points :
- Musculoskeletal Diseases
- Occupational myalgias
- Post-traumatic hyperirritability syndrome
- Joint dysfunction (osteoarthritis)
- Tendonitis and bursitis
- Neurological Disorders
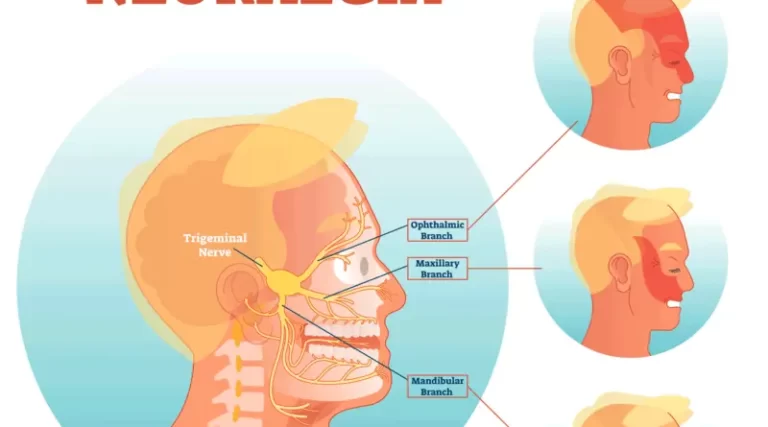
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Sphenopalatine neuralgia
- Systemic Diseases
- Systemic lupus erythematosus (SLE)
- Rheumatoid arthritis
- Gout
- Psoriatic arthritis
- Infections ( bacterial, parasitic, viral, protozoan, and Candida albicans infection)
- Lyme Disease
- Hypoglycemia and Hypothyroidism
- Heterotopic Pain of Central Origin
- Axis II-Type Disorders
- Psychogenic pain
- Painful behaviors
Symptoms of Trigger Points
- A patient commonly asks for help because of a chronic pain state (such as aches everywhere, headaches, TMJ syndrome morning stiffness, tinnitus…), which, in reality, is usually physically far from the active trigger point.
- Muscle weakness or imbalance, changed motor recruitment, besides the affected muscle or in functionally associated muscles.
- Altered in Range of Motion (ROM).
- Painful movement and/or movement that frequently can exacerbate symptoms.
- Migraines, Tension headaches, tinnitus, and temporomandibular joint problems… as accompanying symptoms.
- Postural deformity and compensations.
Diagnostic Procedures
Palpation
Palpation is the last present standard for the diagnosis and examing of TrPs and is the standard front of which new diagnostic methods are assessed. nevertheless, interrater reliability estimates for palpation are distinct largely, suggesting palpation is unreliable.
Imaging
Imaging modalities have currently shown a potential to indicate TrPs :
Sonoelastography was able to detect contrast between clinically relevant clusters and identify TrPs. It is a theory that vibration sonoelastography and shear wave elastography has more steady results because of their use of mechanically-induced stimuli.
Anamnesis
- Anamnesis (a patient’s account of their clinical history) must be precise. The patient should be asked about fibromyalgia, its existence of it, and the history of the family disease.
- Also, the patient must be asked about his physical and daily routine in the present and in the past as less exercise and a more sedentary life may be a pathogenic cause. besides, (chronic) muscle overactivity, daily stress, medications (and their overuse), and sleep disturbances must be asked about and examined in detail.
Examination
- In 2018, an international Delphi panel revised a Trigger point diagnostic approach & proposed that a minimum of two of the following criteria must be present: a hypersensitive point a taut band, and referred pain.
- Palpation must be performed by moving the digits forward and backward, perpendicular to the muscle fibers. Instead, certain muscles can be palpated by the use of a pincer grip.
- Once the taut band has been identified, the hypersensitive point must be located by gently compressing the point across the taut band. Alongside palpation, clinicians must ask the following: ‘Which of the following point is the most painful?’, ‘Is this pain part of your common complaints?’ Does the pain refer distinctly from the point that I am compressing?’
- An affirmative response to the first question confirms the hypersensitive point criteria.
- An affirmative response to the 2nd question clears the pain recognition criteria; and finally, the 3rd question clears the existence of referred pain.
Outcome Measures
- Fischer has proposed the use of the pressure threshold meter known as an algometer, as a means of the quantitative documentation of the TrPs, and for quantifying the effects of the physical therapy treatment.
- Pressure pain threshold and visual analog scale (VAS) point were the result measures more used in the analyzed trials.
- ROM also may be a result measurement for evaluating therapy.
Medical Treatment of Trigger Points
Medications
- Milder forms of pain may be relieved by over-the-counter medications example Tylenol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) example ibuprofen, aspirin, and naproxen.
- Both acetaminophen and NSAIDs decreased pain caused by stiffness and muscle aches, and additionally, NSAIDs reduce inflammation (swelling and irritation).
- If over-the-counter drugs do not give relief, a doctor may prescribe muscle relaxants, anti-anxiety drugs (Valium), antidepressants (Cymbalta), NSAIDs for example Celebrex, or a short course of powerful painkillers (codeine), hydrocodone and acetaminophen (Vicodin).Trigger Point Injection (TPI)
- This is a procedure of entering a small needle into the patient’s active TrP. The injection consists of a local anesthetic or saline and may consist of a corticosteroid. With the injection, the TrP is made inactive and the pain is elevated.
- frequently, a short course of treatment will result in constant relief. Injections are performed by a physician and commonly take a few minutes. Several places may be injected in one visit. If a patient has an allergy to some drug, a dry-needle technique (involving no medications) can be performed.
Physical Therapy Treatment in Trigger Points
- If possible, everyday-life factors that elect the emergence of a TrPs should be prevented or reduced, Posture training and awareness related to postures and lifestyle, Passive stretching and Foam Roller stretching, sometimes a day, Self-massage, times a day, and especially Deep Stroking
- Massage done rhythmically and in only one direction, Strengthening: started only isometric and then isotonic exercises, Ischemic Compression Technique – the term has been performed to explain treatment in which ischemia is induced in the TrPt zone by applying constant pressure.
- However, this principle is questionable, since the nucleus of the TrP is intrinsically present in important hypoxia.
- Simons explains a parallel treatment modality without the need to induce additional ischemia in a TrP area (TrPPressure Release).
- The goal of this technique is to free the contracted sarcomeres within the TrP.
- The amount of pressure applied should suffice to elicit gradual relaxation of the tension within the TrP site, without resulting pain.
- however, both techniques give imitate significant improvement in the range of motion after treatment.
- Taping Technique, Spray and Stretch Technique by the use of ethyl chloride spray,
- Manual Lymphatic Drainage (MLD), since the existence of TrPs obstacle lymphatic flow,
- Other types of proprioceptive neuromuscular techniques: Post-Isometric Relaxation (PIR), Reciprocal Inhibition (RI), Contract-Relax/Hold-Relax (CRHR), Contract-Relax/Antagonist Contract (CRAC), few certain techniques for example Neuromuscular Technique(NMT), Muscle Energy Technique (MET), and Myotherapy (MT), Ultrasonography, Hot and Cold packs, Diathermy- Tecar therapy, Iontophoresis, Laser.
FAQ
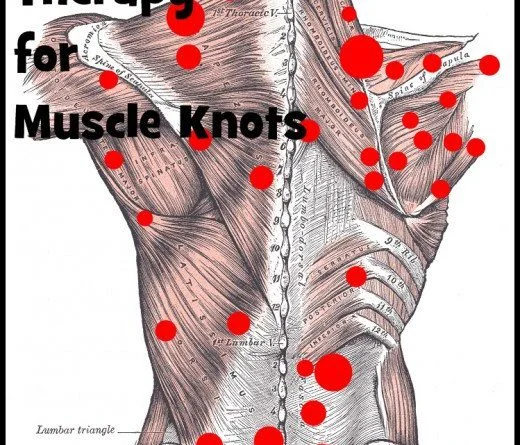
Trigger points feel like small marbles or knots just beneath your skin. When pressing on the trigger spot, most people feel no pain or discomfort. Sometimes, trigger points become very sensitive, and few people feel significant pain in places where they have trigger points.
Trigger points developed in the myofascial, mostly in the center of a muscle belly where the motor endplate enters (primary or central TrPs). Those are palpable nodules within the tight muscle of the body at the size of 2-10 mm and can demonstrate at any distinct sites in any skeletal muscle of the body.
You can use massage techniques to heal muscle knots. Massage therapy enhanced circulation and improves blood flow. That help to improve muscle function and help loosen your tight muscles. This helps to relieve pain and stiffness.
Physical therapists are well-trained to feel where knots occur by looking for tension in the back, neck, and shoulders. They find this tension and release it by applying deep compression with their thumb, digits, or elbow, and holding for 20-30 seconds.
Physical therapists are well-trained to feel where knots occur by looking for tension in the back, neck, and shoulders. They find this tension and release it by applying deep compression with their thumb, digits, or elbow, and holding for 20-30 seconds.




3 Comments