“Knots” and “Trigger Points”: How to Untie the Knot and Be Active in your Treatment
Ouch! That feeling again when you get another knot in your back. Why do those come around to bother me? What are they? Why do I get knots in my back? What can I do to get rid of them? These knots are also known as “tender points” or “trigger points” and will be the focus of this narrative. We will identify what a trigger point is, why they happen, what conditions they are associated with, and the best available evidence for treatment.
What is a Trigger Point?
Myofascial Tender or Trigger points (TrPs) are hyperirritable spots in skeletal muscle that present as palpable nodules (AKA “knots”) in the muscle. Common locations include the mid back, neck, and shoulder blade, however trigger points can arise anywhere in skeletal muscle. Tender points are defined as an isolated point of pain located in the muscle belly of skeletal muscle. On the other hand, trigger points tend to refer or radiate pain elsewhere in the body.
To date, there is no official diagnostic test for myofascial trigger points, therefore diagnosis is made based on the patient’s history paired with palpatory exam findings gained by physicians, physical therapists, or other primary health care providers.
A map of potential trigger points
Why do Trigger Points Happen?
Generally speaking, the reason why trigger points arise is largely unknown. There are multiple theories as to why they may manifest, including theories regarding fascial restrictions over skeletal muscle, problems with blood flow and tissue perfusion just to name a couple. What we do know is that myofascial trigger points are typically associated with other injuries and/or pathologies. There are many reasons why trigger points can arise and cause pain, including:
Muscular Weakness
Neck/Back Pain,
Nerve Irritation/Damage
Joint Hypermobility or Hypomobility
Postural Faults
Stress and Stress Related Disorders
Sleep Disturbances
And many more
Thankfully, trigger points are usually very benign and do not persist, but in some cases they may impact one’s quality of life and daily functioning.
How do you treat Trigger Points?
One thing that I always stress to my patients, SPTs, and interns is that trigger points and tender points are more often a symptom rather than a standalone diagnosis. In other words, as we discussed above there is likely a cause to the trigger points and “knots” that can be addressed.
Manual Therapy
Various manual therapy techniques can be used to address trigger points both locally (applied directly to the knot) or regionally (addressing the root cause and/or above and below the area involved). Below we highlight some treatment strategies that may help you with your knots:
Joint Mobilization/Manipulation
Based on our assessment, spinal manipulation may be indicated to address your pain. Some techniques include manipulation to the thoracic spine, cervical spine, and/or the cervicothoracic junction (CTJ). Furthermore, if deficits are noted in the shoulder girdle or scapular region, joint mobilization techniques may also be appropriate.
STM and Trigger Point Release
Although this can sometimes be uncomfortable, “Trigger Point Release” such as ischemic compression can help decrease pain locally at the trigger point. This is done by a physical therapist or other practitioner, but can also be self taught as we discuss later in this narrative.
Cupping Therapy, Dry Needling, and Taping
Other adjunctive treatments such as cupping, dry needling, and kinesiotaping are gaining popularity and may help with trigger point pain in conjunction with exercise, education, and other manual therapy interventions.
Therapeutic Exercise
Good physical therapists understand that treatment should always be ACTIVE. After applying skilled manual therapy listed above, we can use this new window of opportunity to train specific muscles, self mobilize the spine and/or other peripheral joints, and educate our patients on a home exercise program (HEP).
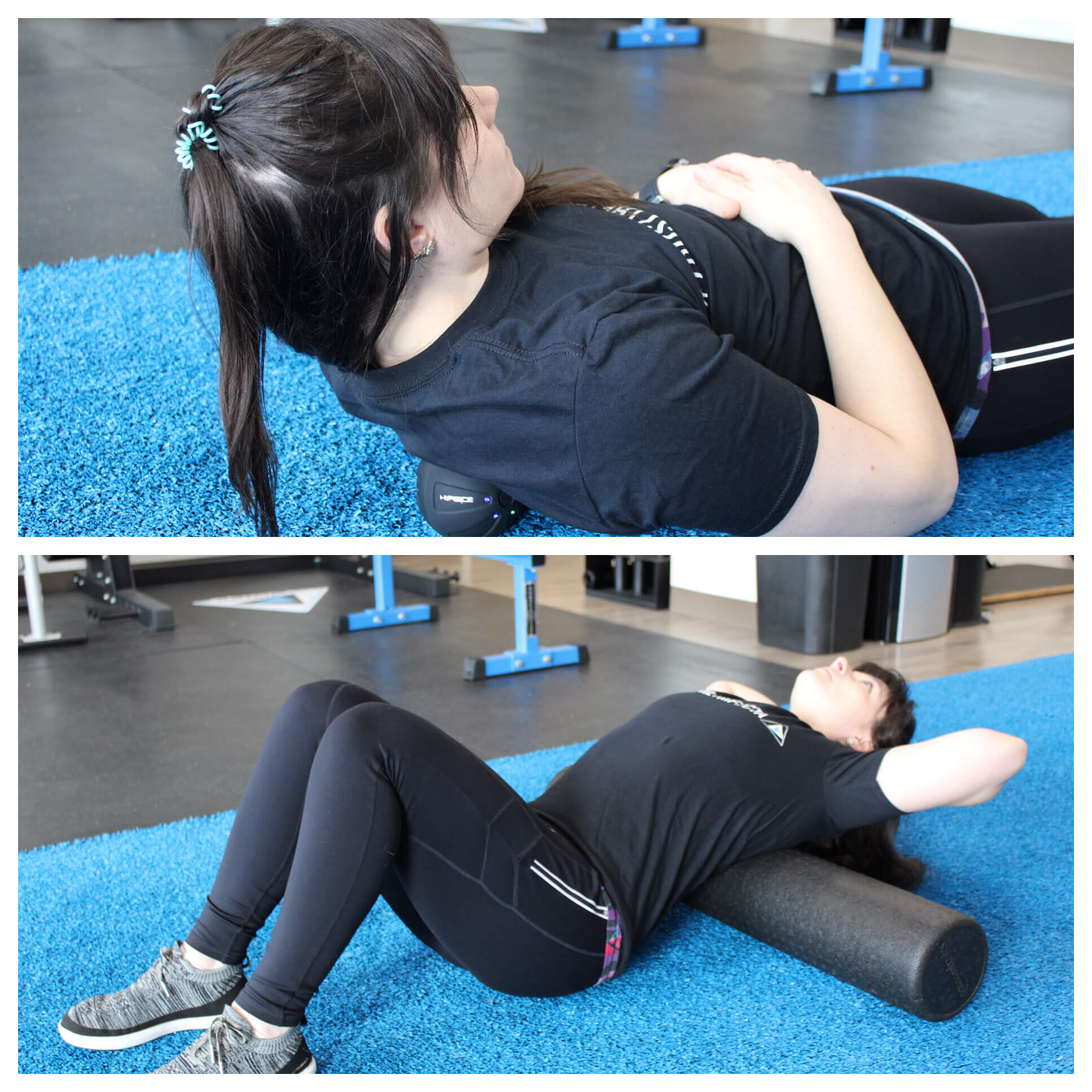
Self Mobilization
After applying manual therapy, specific self mobilization techniques such as those shown below can help capitalize on the techniques applied by your PT. This can include, but is not limited to, thoracic extension mobilizations, foam rolling, and self-ischemic compression with a lacrosse ball or other device such as the HyperIce Minisphere
Periscapular Strengthening
It is CRUCIAL to address the underlying causes that could be leading to your knots and trigger points. Sometimes this involves strengthening the muscles that surround and move your scapulae and your shoulders. These “postural muscles” are an important part of living a pain free life! Below are some examples or exercises that may help address the muscle imbalances found on your examination:
Neurodynamic Stretching/Flossing
If indicated, your physical therapist may apply specific neurodynamic techniques to address tension in the nervous system and provide you with home flossing exercises to further improve upon this exam finding.
Conclusion
The goal of this narrative was to briefly highlight the nature of and treatment of myofascial trigger points. This is a common complaint that I see in the clinic and something that impacts many people each and every day. I hope that this information sheds some light on this often challenging topic. If you have any questions about this topic or any other topic, feel free to contact myself or one of our other residency-trained specialists!
Be well,
Dr. Justin Hanus, PT, DPT, CSCS
Candidate for Orthopedic Board Certification (OCS)
jhanus@trifectatherapeutics.com
References:
Fernández-de-las-Peñas, C., & Dommerholt, J. (2018). International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study. Pain Medicine, 19(1), 142-150.
https://www.physio-pedia.com/Trigger_Points
Simons DG, Dommerholt J. Myofascial trigger points and myofascial pain syndrome: a critical review of recent literature. Journal of Manual & Manipulative Therapy. 2006 Oct 1;14(4):125E-71E
Are you interested in our services at Trifecta Therapeutics, but live too far away from our facility? Schedule a telehealth visit!